The Role of Technology in ACL Rehabilitation: Mick Hughes
Available in:
EN
Mick Hughes is an Australian Physiotherapy Association Titled Sports & Exercise Physiotherapist with dual qualifications in Physiotherapy and Exercise Science.
Since 2016, Mick has focused his time and passion in specialising in ACL rehabilitation and has helped co-author the Melbourne ACL Rehabilitation Guide. He is a founder of Learn.Physio and has presented workshops on ACL rehab countless times around the world.
He currently works at North Queensland Physiotherapy Centre, and was previously Head Physiotherapist and High Performance Manager for the Collingwood Magpies Netball Team in the National Netball League and consulted at The Melbourne Sports Medicine Centre for 6 years.
A couple of years ago, VALD’s Mark Opar interviewed Mick on Force Plates in Clinical Practice. Since then there has been a lot of progress in ACL rehabilitation and criteria-based-return-to-sport testing, with particular focus on single leg vertical jump performance. So we thought we would check in with Mick again to hear his clinical insights on using objective measurement technologies in ACL injuries.
When were you first exposed to objective measurement technologies such as force plates and handheld dynamometry?
I was first exposed to force plate technology during my placement for my Masters of Sports Physiotherapy program at the Melbourne Storm NRL club. During this placement, I observed the sports science and physiotherapy departments assess players in a variety of jump tests and hop tests to evaluate their readiness to train, assess fatigue from games and monitor progress through rehabilitation and injury. This clinical experience showed me how we could integrate sports science technology into a physiotherapy clinical setting to help manage the patients I was seeing.
Regarding handheld dynamometry devices, I had been exposed to them early in my career, and they were something that I was more familiar with. However, I had not been using them consistently until I started seeing a high volume of ACL patients and saw how more experienced clinicians were using handheld dynamometry to assess and progress their ACL patients. This was a valuable lesson for me, as it showed me how to use these technologies to help my patients more effectively, rather than simply referring them for isokinetic testing.
When did you first start using VALD Technologies and why?
I started using VALD Technology in late 2020 when we first purchased the NordBord for our Melbourne Sports Medicine Clinic. Subsequently, we also purchased the ForceDecks. Both of these testing devices were useful in assessing my ACL patients, and my clinical directors saw the value in using both testing devices across many different lower limb pathologies outside of ACL patients and hamstring testing. More recently, I have been able to use the DynaMo to routinely and conveniently test quadriceps strength in my ACL patients and track and monitor progress throughout rehab.
Spanning across your career, what are the key differences in your current approach to rehabilitating ACLs now that you have objective measurement technology available in clinic?
I guess the big difference – now that I have testing systems such as the ForceDecks and DynaMo – is that my approach to rehabilitation is very direct. I’m looking more for impairments and addressing those impairments because I can accurately measure them.
For example, without the use of the DynaMo and NordBord, I was never really able to identify quadriceps weakness or hamstring weakness reliably. Knowing that both of those muscle groups have an influence on ACL rehab outcomes, I’ve been able to target those muscle groups better. As a result, my exercise rehabilitation is much more targeted than it was before.
I guess the big difference – now that I have testing systems such as the ForceDecks and DynaMo – is that my approach to rehabilitation is very direct.
Building on that, ForceDecks has been a game-changer for me. I’m now able to clearly identify problems with patients in ACL rehabilitation during jumping, landing and hopping that traditionally I was not able to identify. I would not be able to get that information from a single-leg hop for distance test, nor any other traditional horizontal hop test.
ForceDecks technology clearly identifies a patient who may have a landing issue by identifying if they are offloading their ACL limb and forcing the healthy limb to accept more force when landing. Conversely, in a single-leg vertical jump measure, I can now accurately identify if there are vertical power issues between limbs.
This is something I’ve never been able to ascertain before until ForceDecks, which now fits easily into the clinical environment.
ForceDecks has been a game-changer for me. I’m now able to clearly identify problems with patients in ACL rehabilitation during jumping, landing and hopping that traditionally I was not able to identify.
What are some of the key tests and metrics used in ACL rehabilitation for return to sport?
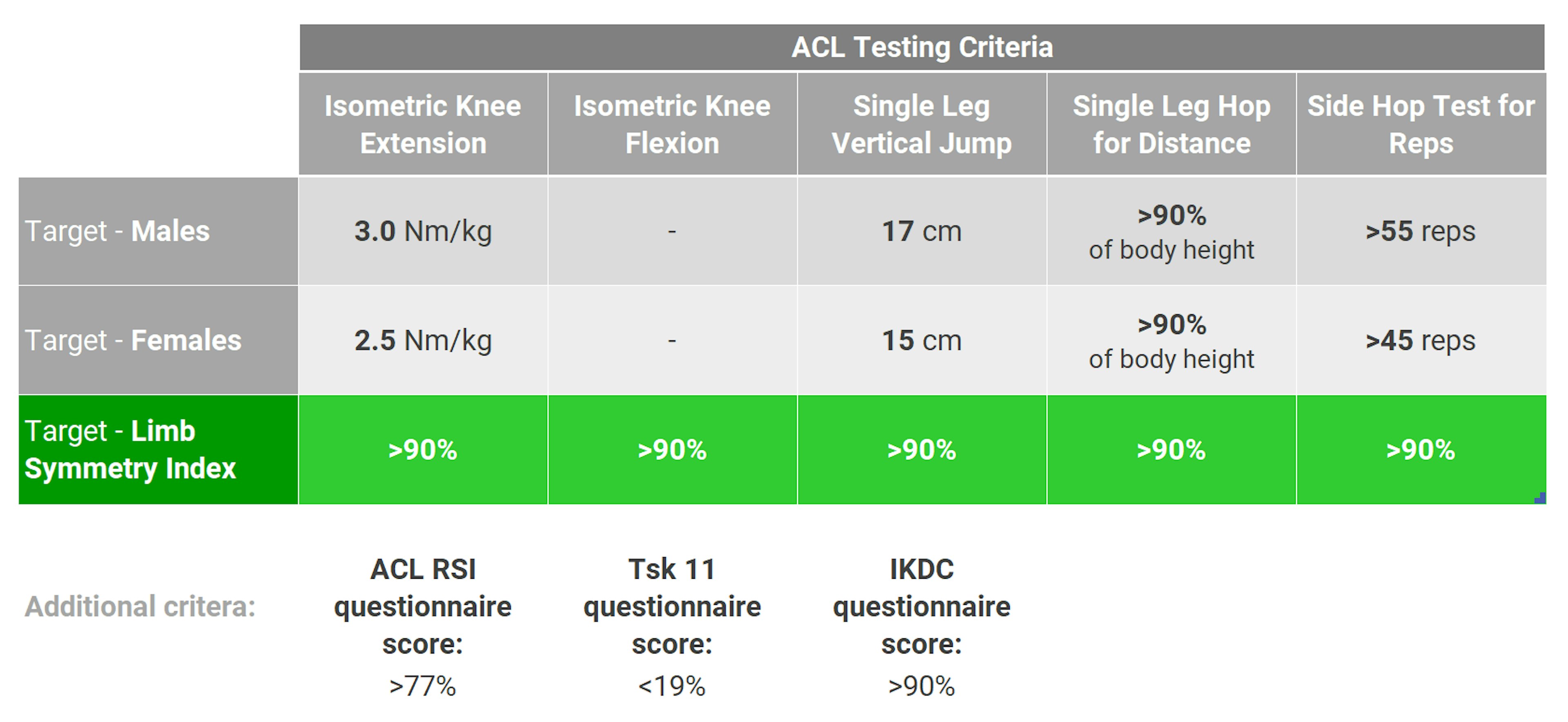
I look at a range of criteria including strength, power, asymmetry, and validated patient reported outcome measures. The table below summarises the key tests as well as some benchmarks I use to help inform my return to sport decisions.
What tests would you do preoperatively?
For preoperative ACL patients, we would test the following objective measures prior to the patient having a reconstruction, that we could use for return to sport decision-making later:
- Quadriceps strength test on the healthy leg.
- Single leg hop for distance on the healthy leg.
- Single leg vertical jump on the healthy leg.
Using the healthy leg as a reference point prior to the operation allows us to set a benchmark for the patient, which will likely be their strongest and most powerful result for the next 6 to 12 months while they are in recovery. If we can estimate how strong and powerful their ‘normal’ is (using the healthy leg as a good reference point) it allows us to make better decisions when they are 9 to 12 months post-op.
I summarised this paper where they used estimated pre-injury capacity scores of the healthy leg and found that it was a much more sensitive way to determine readiness to return to sport, rather than using the traditional limb symmetry index score.
Using the healthy leg as a reference point prior to the operation allows us to set a benchmark for the athlete. If we can estimate how strong and powerful their ‘normal’ is … it allows us to make better decisions when they are 9 to 12 months post-op.
In respect to metrics, I’m simply looking to get peak values of both:
1. Single leg knee extension strength (measured isometrically at 90 degrees of knee flexion using DynaMo)
2. Single leg vertical jump maximum height.
Have you noticed a difference in how patients approach rehab now that you use objective measurement technology?
I have definitely noticed a difference in the last few years with regular testing of ACL patients using DynaMo, ForceDecks and NordBord. The patients, I feel, have bought into rehabilitation better and are excited about reviewing their progress every month, knowing that they will be tested. Having these regular monthly check-ins enables us to motivate and progress rehab in a clear and concise way.
Every time we review a patient, I am able to test and look for asymmetries or weaknesses within the patient so we can address these impairments. This helps the patient get stronger and more powerful each time I review them. It really enables me to build a clear and concise rehab program to address these impairments so we can get the patient back in a timely fashion and in the best possible way to reduce future injuries.
The patients have bought into rehabilitation better and are excited about reviewing their progress every month, knowing that they will be tested. Having these regular monthly check-ins enables us to motivate and progress rehab in a clear and concise way.
How has objective data played a role in communicating with patients or those involved in their care?
An example I can think of is a recent patient who had undergone ACL reconstruction surgery and was experiencing significant pain, swelling, and dysfunction six months post-op. When the patient visited me, they reported a lack of organization and regular assessment during the first six months of rehab, with rehabilitation largely progressing via arbitrary time points.
When I was able to objectively test the patient’s isometric hip and knee strength, I was clearly able to see why the patient was struggling to run, jump, and hop at six months post-op. The objective measurements showed a 40% strength difference between limbs for both quadriceps strength and hamstring strength tests, with both of those strength values being insufficient to handle the demands of running, hopping, and jumping. With this information, I was able to provide feedback to the patient’s surgeon, regular physiotherapist and strength and conditioning coach.
When I was able to objectively test the patient’s isometric hip and knee strength, I was clearly able to see why the patient was struggling to run, jump, and hop at six months post-op.
With this new information, we were able to formulate a more objective plan targeting the impairments of quadriceps and hamstring strength impairments. This program would enable the patient to better tolerate running, jumping, and hopping in the future. Within two months of targeted strengthening exercises in conjunction with managing the knee swelling, the patient was able to tolerate running, jumping, and hopping again.
Without the data insights from objective measurement technology being readily available, this patient ordinarily might have had to go down a medicalised road to manage her symptoms. By clearly being able to identify and address the specific weaknesses, we were able to have a really good result and outcome.
Any final words of advice for those involved in ACL injury prevention or rehabilitation?
My big advice here for clinicians who are managing ACL patients is to take regular objective measures of your patients throughout rehab. This should start from their first presentation to you (ideally pre-operatively) and continue right through to return to play and discharge.
My big advice here for clinicians who are managing ACL patients is to take regular objective measures of your patients throughout rehab. This should start from their first presentation to you (ideally pre-operatively) and continue right through to return to play and discharge.
We want to be testing and assessing their healthy leg pre-operatively and then postoperatively. We want to be taking regular objective measurements all the way throughout rehab and, importantly, discharging the patient back to competitive sport via objective testing systems rather than time since surgery or a clinical examination or even simply manual muscle testing. These are not good enough to determine a patient’s readiness to return to sport. We need objective strength data of quad and hamstring strength, and we also need objective data on vertical jump, horizontal hop, and reactive strength index.
If you would like to know more about how to integrate VALD’s human measurement technology into your organisation to help with the engagement of your clients, please reach out here.
